Learn about Perforator Vein Reflux
How Do Perforators Contribute to Varicose Veins?
At the Vein Treatment Center, Dr. Karamanoukian has expertise in traditional perforator surgery - ligation via open techniques, as well as ablation with endovenous technology. You will read herein the definition of venous insufficiency, perforator reflux, perforator vein reflux, perforator venous insufficiency, pathophysiology of perforator venous insufficiency, types of perforator veins, videos showing perforator venous reflux disease - videos showing perforator venous reflux disease contributing to healed and active venous stasis ulcers - videos of perforator venous reflux in the thighs, legs, ankles - and so on. We utilize state-of-the art technology to perform these ablation procedures for perforator veins and use the EVLT Never Touch system to perform incision free, suture free, nearly pain free perforator vein treatments atwww.VeinsVeinsVeins.com
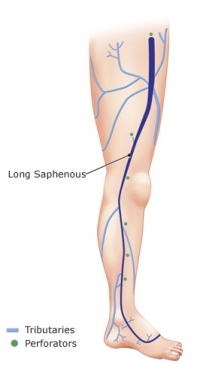 In addition to saphenofemoral reflux and valve incompetence causing symptomatic venous reflux disease involving truncal veins, there are several sites along the greater saphenous vein and lesser saphenous vein where there is potential for branch varicosities and communication with the deep veins of the lower extremities. Free communication as well with deep veins to non-saphenous veins in the legs can also occur with perforator venous insufficiency. These include the perforator veins. Perforator veins allow communication between the superficial venous system and deep venous system of the legs. Superficial veins include the great saphenous vein and its branches and the lesser or short saphenous vein and its branches, as well as other non-named superficial veins in the legs. The deep veins of the legs include the common femoral vein, femoral vein (previously called superficial femoral vein), popliteal vein, anterior tibial vein, posterior tibial vein and peroneal veins, among others.
In addition to saphenofemoral reflux and valve incompetence causing symptomatic venous reflux disease involving truncal veins, there are several sites along the greater saphenous vein and lesser saphenous vein where there is potential for branch varicosities and communication with the deep veins of the lower extremities. Free communication as well with deep veins to non-saphenous veins in the legs can also occur with perforator venous insufficiency. These include the perforator veins. Perforator veins allow communication between the superficial venous system and deep venous system of the legs. Superficial veins include the great saphenous vein and its branches and the lesser or short saphenous vein and its branches, as well as other non-named superficial veins in the legs. The deep veins of the legs include the common femoral vein, femoral vein (previously called superficial femoral vein), popliteal vein, anterior tibial vein, posterior tibial vein and peroneal veins, among others.
">Video about Perforator Venous Reflux Disease by Dr Karamanoukian:
So what does the "perforator" terminology mean? It means that the vessel "perforates" the aponeurosis of the muscle, giving it the name 'perforator vein'. The aponeurosis is fascial tissue that invests or envelops muscle groups and binds these muscle groups to other muscle groups or to bone.
According to Dr. Alberto Caggiati (Rome, Italy), perforator veins were not identified nor described by the 'fathers of vascular anatomy and physiology' in the 16th and 17th centuries. Perforator veins were first reported in the Anatomische Tafeln zur Beforderung der Kenntniss des menschichen Korpers (Weimar, 1794-1803), the main work of the German anatmist Justus Christian von Loder (1753-1832).
The superficial veins communicate with the deep veins via perforator veins. If you imagine the two legs of the letter "H" , the perforator vein is the connection between the two legs of the letter "H". That "connection" is the part that perforates the muscle fascia and connects the deep veins to the superficial veins.
There are many perforator systems in each extremity. Sometimes, these perforators are causes of "failure" of treatment after "successful ablation" or "successful sclerotherapy" sessions. This means that cosmetic procedures done by untrained professionals for varicose veins and reticular veins and spider vein complexes can fail if there is underlying perforator venous reflux disease. The treated varicose veins or spider veins can recur if the perforator reflux is not treated (see below). As well, trophic changes in the skin in patietns with venous disease, namely hyperpigmentation and lipodermatosclerosis can progress to venous stasis uceration if perforator venous reflux disease remains untreated. Dr. Karamanoukian has expertise in treating perforator venous reflux with traditional (open surgical techniques) or with EVLT microfiber laser technology.
There are valves within these perforator veins which can also become incompetent and cause branch vein varicosities throughout the lower extremities - at the level of the thighs, knees, lower legs, ankles and feet. However, they are most common in the legs, below the knees.
Perforator veins typically have one to three valves. These are bicuspid valves. Bicuspid valves have two valve cusps. This is unlike the tricuspid aortic heart valve (3 cusps, looking like the 'Mercedes Benz' insignia). These bicuspid valves of the perforator veins are oriented to allow blood to go in one direction, from the superficial veins to the deep veins. The unidirectional blood flow in these perforator veins is also maintained by the oblique course of the perforator veins through the muscle and aponeurosis (see above for definitions). As shown in the cartoon below (taken from Jean Francois Uhl, MD) that perforator veins are direct (with an oblique course) or indirect, i.e. through an arborizing network of veins. The latter gives an added degree of complexity to an already complex network of veins that result in perforator based venous reflux disease.
Video 1 :
">Perforator Venous Reflux Disease and healed venous stasis ulcer by Dr. Karamanoukian of
www.VeinGuide.com
Video 2 : Dodd's Perforator Venous Reflux Disease (mid thigh perforator vein) by Dr. Karamanoukian of www.VeinGuide.com
Video 3 : Cockett's II Perforator Venous Reflux Disease Treated by EVLT laser by Dr. Karamanoukian of www.VeinGuide.com
The average number of perforator veins per extremity is highly variable and reported in the literature to be as many as 155! Obviously, not all of these are clinically important, but some can cause significant morbidity to the patient. They are thought to play a fundamental role in the development of varicose veins in the lower extremties.
A recently published study from Zagreb, Croatia (Croat med J 2005; vol 46: page 245-251) showed that deteriorating venous insufficiency of the great saphenous vein correlates with the number of incompetent perforator veins per leg as well as the diameter of the perforator veins. This implies that the presence of perforator venous reflux represents a significant factor in the development of venous reflux disease in the great saphenous vein. Other conclusions also derived from this seminal study are that with the deterioration of CEAP grade, a scoring system for venous disease, there is an increased capacity for blood volume to be expelled down a pressure gradient through both dilated low-resistance perforator veins that are incompetent (leaky) and the incompetent greater saphenous vein. As such, if surgery is limited to the greater saphenous system alone, neglecting perforator vein insufficiency, saphenous vein treatment alone would be incomplete treatment. Perforator surgery should be added after an interval time and after re-evaluation by Duplex scanning, especially if there is associated symptoms or trophic changes in the skin (residual stasis dermatitis, hyperpigmentation of the skin, lipodermatosclerosis, or active venous stasis ulcers).
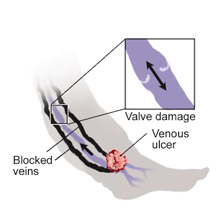
Why is perforator surgery important? It has been estimated that in patients who develop chronic venous insufficiency, 4% will progress to develop venous stasis ulcers. That is a high number, signifying that 1 in 25 people who have chronic venous insufficiency will develop these venous stasis ulcers.
As well, a study published in the European Journal of Vascular and Endovascular Surgery (volume 21: page 458-460) demonstrated that patients with recurrent varicose veins have both a higher prevalence and a greater number of incompetent perforating veins than patients with primary varicose veins. As such, the importance of addressing and treating perforator venous reflux disease cannot be underscored.
Treatable superficial venous reflux disease is associated wtih perforator venous reflux disease in approximately 77% of patients with venous stasis ulcers and 57% of patients with trophic changes in the legs. The conclusion from this data is that patients with venous stasis ulcers and trophic changes with combined superficial venous reflux disease and perforator venous reflux disease benefit from treatment of perforator veins.
The distribution of perforator veins increases in density and one approaches the ankle - they occur in a ratio of 8:1, with 8 times more perforator veins in the lower leg, ankle and foot than in the thigh. More important that the sheer number of these perforator veins is the number of incompetent perforator veins . When they are incompetent, perforator veins reach diameters of 5 mm or more and can have large volume flow, feeding an array of varicose veins above the fascial layer of the muscle.
Image taken from gecommunity.gehealthcarecom from the work of Mira Katz PhD, RVT - accessed on November 14, 2009
The gaiter areas are the areas where skin changes and venous stasis ulcers are most likely to occur - these areas are where the most prominent perforator veins are likely to be found. perforator vein incompetence in these gaiter areas have been shown to increase ambulatory venous pressures above 100 mm Hg (venous hypertension), a phenomenon which has also been referred to "ankle blow-out" syndrome in the gaiter areas. The combination of incompetent perforator veins and resultant venous hypertension over time causes damage to capillaries in the skin and nd subcutaneous capillaries, allowing protein rich fluid and red blood cells to escape into the subcutaneous tissue around the ankle. The effect is that the subcutaneous tissue becomes fibrotic and skin pigmentation results from hemosiderin deposition.
Watch New Video about Perforator Venous Reflux Disease (Cockett's) by Dr Karamanoukian:
Watch Video Clip of VNUS Closure RFS Procedure for Perforator Venous Reflux:
&feature=related
The clinically important perforator veins are in the thigh (Dodd's and along Hunter's canal), calf (soleus and gastrocnemius types), medial leg below knee (Boyd's), lateral (outer) leg (peroneal) and Cockett's. The Cockett's type is the most recognized and occurs within 20 cm of the ankle. The tenet of the constancy of Cockett's perforating vessels does not hold against anatomical studies. They perforate the fascia at various levels as their relationship to Linton's line also vary. They occur within a "lane" of 3 cm along the line previously described by Linton. the first set occurs within 6-10 cm of the ankle; another set of Cockett's perforators occur at 13.5 cm to 15 cm of the ankle; a third set of Cockett's perforators occur from 18 cm to 20 cm of the ankle; the fourth and final set of Cockett's perforators occurs between 24 and 25 cm of the ankle along Linton's "lane". An experienced phlebologist can locate these important perforators and deal with them in a manner to heal venous stasis ulcers and also to treat symptomatic varicosities arising from these refluxing perforator veins.

image of marked Cockett's perforator veins for surgical ligation taken from circulationforum.com on January 11, 2009 (see above)
There are also recognized perforater veins of the foot (medial and anterior and lateral) that can cause significant morbidity when they are incompetent. Peroneal perforator veins are also the 'lateral calf perforators' and are found 5-7 cm (Bassi's veins) and 12-14 cm from the lateral ankle. The peroneal perforators connect the lesser saphenous veins with peroneal veins.
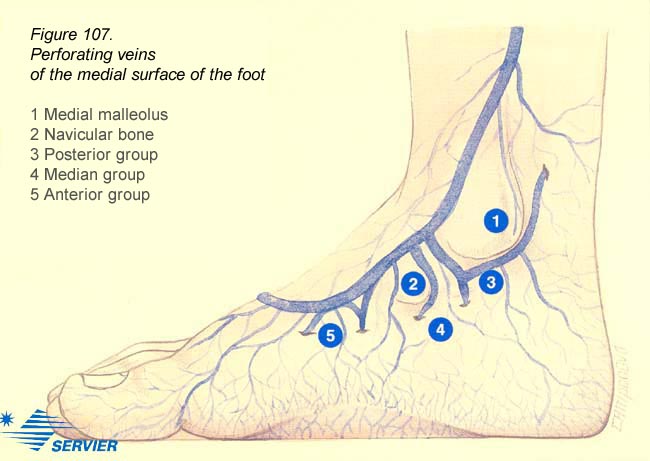
image taken from phlebologia.com on January 11, 2009
So, how does one get varicose veins after the VNUS Closure procedure? This is a very good question and as the carton image below shows, perforator veins below the ablation segment of the great saphenous vein using VNUS Closure contribute connections to the superficial system of veins and thus give rise to surface varicosities that become inflamed. Clinically, patients present with phlebitis and all of the symptoms associated with inflamed cords of varicose veins: aching, pain, heaviness, tiredness, fatigue, itching, burning, cramping, throbbing, restless legs and swelling (see image below):
image taken from dssurgery.com on November 14, 2009 (image changed on this date from prior image)
Perforator Vein Reflux Treatment
In the past, surgery designed to divide the perforating veins, such as Cockett and Linton procedures, were associated with considerable morbidity. The recently developed technique of subfascial endoscopic perforator surgery (SEPS) has allowed perforating veins to be divided effectively but with considerable incisions and down time. As importantly, utilization of minimally invasive techniques that have been developed by Dr. Karamanoukian using expertise he has gained as a cardiac surgeon have revolutionized these techniques into smaller incisions that allow optimal wound healing with minimal morbidity. Treating these perforator veins with microfiber laser technology has further enhanced the minimally invasive nature of these procedures for venous insufficiency involving perforator veins. Patients wear an ace bandage over the area for 4 hours only, remove them and resume all activities immediately. There are no cuts, no sutures, no down time with perforator vein EVLT laser procedures!
There is hope! New technology using radiofrequency ablation and EVLT Never Touch allows for obliteration of these perforators under local anesthesia in an ambulatory office setting. New EVLT micro laser fibers allow for obliteration of these perforators in the thigh, leg, and ankle. These ablative technologies are used selectively at the Vein Treatment Center to achieve the desired effect in healing venous stasis ulcers and treat recalcitrant varicosities that are not responsive to microphlebectomy or ablation of truncal venous insufficiency involving the great and Small saphenous veins.
Even more significant technology uses VenaCure EVLT Never Touch laser technology which we use on a routine basis to obliterate perforator venous reflux disease in patients with debilitating venous disease including perforator venous reflux disease and venous stasis ulcers. The VenaCure EVLT laser technology is the currently favored technology to treat perforator venous reflux at the Vein Treatment Center.
Patients with venous ulcers in the legs may well have perforator reflux and can be screened by clinical examination at the time of consultation using the Brodey-Trendelenberg test and the Bracey variation of this test. They are confirmed by the presence of fascial defects on examination and verified by an ultrasound and duplex venous study. We have clinical expertise at the Vein Treatment Center to diagnose and treat perforator veins and reflux originating from perforator veins. Minimally invasive techniques can accomplish ligation of these perforators to help heal stasis ulcers and get you back to your routine.
Schedule your treatment
The surgeons at the Vein Treatment Center have the technology and equipment to diagnose and treat perforator reflux disease. To schedule an ultrasound screening examination, contact us at (716) 839-3638. You qualify for this assessment and perforator treatments even if you have had vein stripping elsewhere or VNUS Closure procedures at other facilities.
Remember that perforator veins can contribute to the development of trophic skin changes (bronzing of the skin and leatheriness of the skin) and also venous stasis ulcers. We have the expertise at the Vein Treatment Center and www.VeinsVeinsVeins.com to treat perforator venous insufficiency - perforator venous reflux disease - perforator reflux - perforator veins.