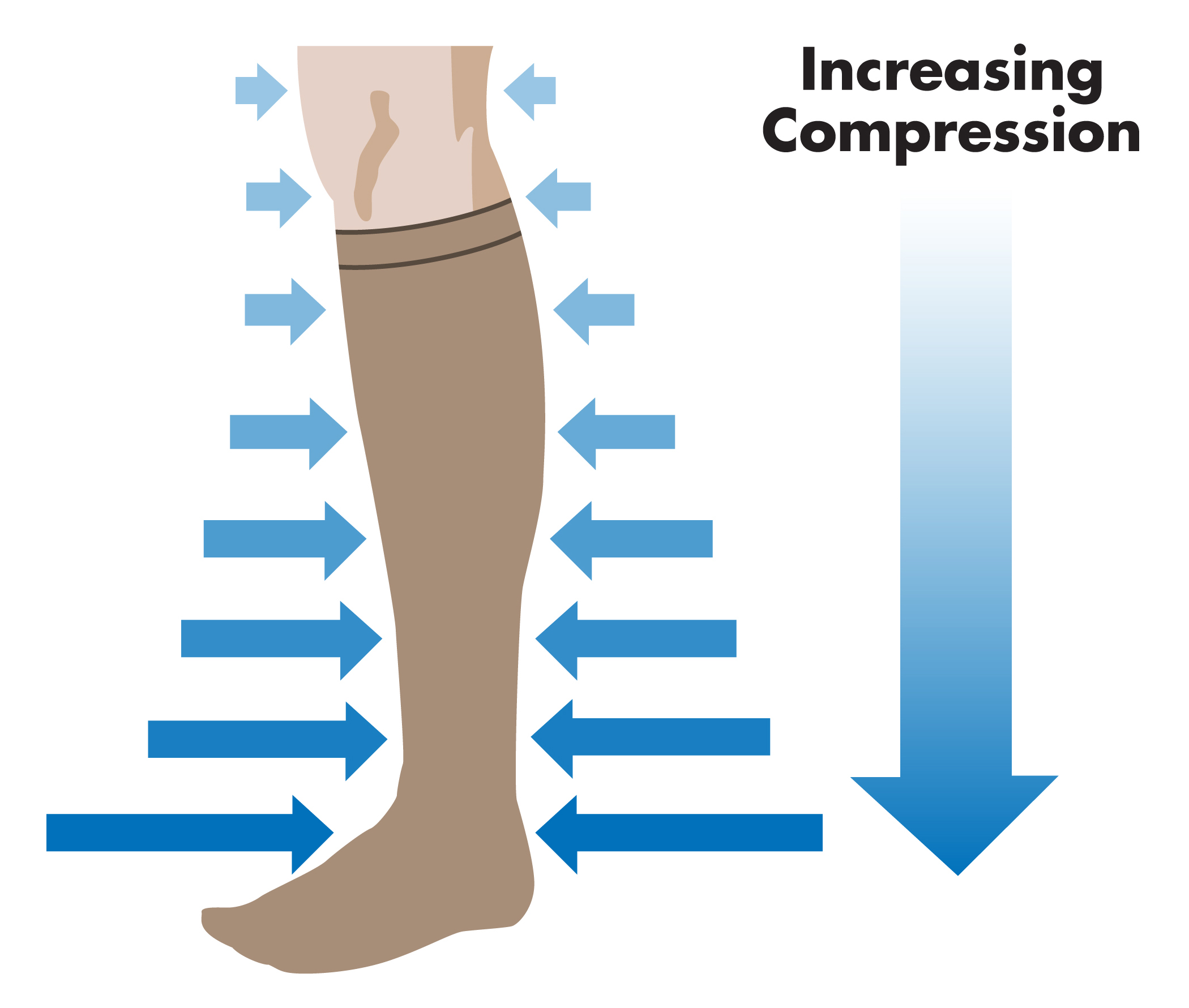
What is graduated compression?
The term graduated compression means that by virtue of graduation (more tapered near the ankle) and larger in the leg and thigh, the graduated compression socks propel blood housed in the leg veins up towards the heart as you walk. Graduated compression stockings are used in patients with chronic venous insufficiency, in patients after surgery to reduce clot formation, after sclerotherapy for telangiectasias and varicose veins, and in patients who want to prevent the development of spider veins, varicose veins or recurrent varicose veins or venous stasis ulcers.
Elastic compression stockings provide stretch in the short and long axis of the leg. They are 'ready made' off the shelf stockings that can be purchased in a drug store or 'made-to-measure' or 'custom made' stockings that are available in specialty stores. Custom stockings use circumference and length measurements of the ankle, leg and thigh to achieve the desired level of compression while at the same time provide patient comfort.
Custom made stockings may be prescribed in patients that are very small or obese, or when there is a difference in the size of one extremity versus the other, as in patients with associated chronic swelling or lymphedema. Most patients, however, do not require 'custom made' compression stockings or compression hose. A doctor can write a special prescription for 'custom stockings' and describe the level of compression desired (15 mm Hg, 20-30 mm Hg, 40 mm Hg and so on). The level of compression and whether or not it should be zippered or not should be specified on the prescription.
Do Patients Wear Compression Stockings ? Compliance with Compression Hose
Compliance is an important factor in wearing compression stockings and compression hose. I often tell my patients when I first see them in consultation : "you can make a decision today as to whether you wear stockings regularly to prevent more vein problems or you will likely come back in the future with new vein problems ... "
Researchers have shown that noncompliance is related to comfort in wearing stockings and/or problems wearing stockings, as some patients feel a sense of restriction and discomfort and pain when they wear stockings. Some of the discomfort is felt at the ankle level where the stockings cause pain because "they get bunched up" or at the level of the knee where they cause pain during ambulation. Others cannot seem to find a pair of stockings that "stay up" and have to constanty pull up the stockings. It becomes important to find a suitable pair of compression stockings that will help the symptoms of venous insufficiency - and that may mean trying different brands and lengths (knee high or thigh high or waist high) that are properly fitted or 'custom made'.
What are the symptoms of venous insufficiency?
- Aching and pain in the legs
- Heaviness of the legs
- Tiredness and fatigue of the legs
- Itching over areas that have stasis dermatitis
- Cramping and throbbing of the legs
- Restless legs
- Swelling of the ankles and legs
How do compression stockings work?
Compression stockings provide external compression and thus limit the ability of distensible veins to distend. Therefore, narrowed varicose veins will limit their ability to hold bold, especially if there is incompetent or leaky vein valves, as in patients with venous insufficiency.
Published studies have also shown that after 15 minutes of wearing compression stockings, there is improvement the oxygenation of the skin (cutaneous oxygenation).
Patients with clinically significant venous insufficiency report improved symptoms when they wear graduated compression stocking - less pain, less heaviness in the legs, less aching of the legs, less tiredness of the legs, less cramping and throbbing of the legs and less leg swelling at the end of the day.
Do compression stockings prevent varicose veins?
Emperic observation in millions of patients show that patients who regularly wear compression stockings are less likely to return with symptomatic venous insufficiency or with new vein problems.
Surprisingly, there are no randomized clinical trials (RCT) showing that compressions stockings prevent the progression of venous disease. Despite this, almost all phlebologists (vein specialists) recommend patients to wear and to continue to wear compression stockings to 'prevent venous disease'.
Do I have to wear compression stockings once my venous ulcer heals?
Once venous stasis ulcers have healed, graded compression stockings have to be worn regularly in order to reduce the likelihood of recurrence. Studies show that grade II compression stocking (30 - 40 mm Hg) are needed and they should be at least to the level of the knee. Compliance in wearing compression stockings is noted to be poor, with only 1 in 2 patients following through with these recommendations. The compliance does improve if there is monitoring by home health care nurses or when there is physician supervision. In a recently published study, recurrence of venous stasis ulcer is 32% at 5 years when compression stockings are worn and 70% at 5 years when compression stockings are not worn.
How is the venous physiology changed with compression stockings?
- Reduction of tissue swelling which has been measured scientifically by ultrasound imaging.
- Softening of skin changes (lipodermatosclerosis) which has been shown by ultrasound imaging and CT scanning.
- Narrowing of veins - blood volume decreases when compression stockings are worn. This has been shown to occur with duplex ultrasound studies and air plethysmography.
- Improved venous flow - venous blood flow velocity (speed) is increased when patients wear compression stockings.
- Shift of venous blood into the deep veins - blood from the superficial veins (veins that are on the surface of the leg) are shifted into the deeper veins (deep and cannot be seen with the naked eye).
- Reduced venous insufficiency - inelastic bandages are more effective than elastic bandages but both reduce the degree of venous insufficiency in the uproght position as measured by Duplex venous ultrasonography.
- Improvement of the microcirculation of the legs has been shown with the use of compression stockings.
- Improved lymphatic drainage
This summary data was abbreviated from a wonderful textbook called Leg Ulcers, Diagnosis and Management, 3rd Edition, Edited by David Negus, Philip Coleridge Smith and John J Bergan (pages 112-115).
5 reasons to wear compression stockings after sclerotherapy - sclerotherapy Buffalo
It is imperative that patients wear compression stockings for a period of at least 3 months following sclerotherapy in order to optimize the cosmetic appearance of the injected areas.
Compression helps in at least 5 ways:
- Compression helps in compression of the vein wall after it is injected, helping the process of producing a fibrous cord, devoid of blood and blood particles.
- Compression reduces the amount of blood residuum in the injected vein.
- Compression reduces the amount of clot formation which contributes to less hyperpigmentation of the injected area.
- Compression stockings after sclerotherapy reduce the likelihood of telangiectatic matting.
- Compression stockings increase deep venous blood flow and clears potential sclerosant that inadvertently gets into the deep venous system.
What do compression stockings do physiologically?
Compression stockings have been shown to be effective :
- Reducing venous volume
- Reducing venous reflux
- Reducing edema
- Reducing ambulatory venous pressures (venous hypertension)
The effects of venous compression on the hemodynamics of the venous system depends on the degree of comprression - 20 mm Hg versus 30 mm Hg versus 40 mm Hg.
Evidence Based Treatments for Venous Stasis Ulcers
- Scientific evidence for the use of expensive dressings is lacking
- The Cochrane collaboration did not find that any dressing is better than another - as long as the are 'no stick' non adherent
- The VULCAN trial did not show any benefit of silver impregnated dressings in regards to ulcer healing
- Compression therapy is the mainstay of any treatment for venous stasis ulcers
- Any compression is better than no compression in the healing of venous stasis ulcers
- Four layer bandages are better in healing venous stasis ulcers than short-stretch bandages
- Multilayer bandages with elastic components are better for healing ulcers than those with inelastic components
- Adjustable compression boots are as effective as compression bandages in healing venous stasis ulcers
Compression Bandages and Stockings - What do they do ?
- reduces distended superfcial veins
- enhances blood flow in the deep veins
- restores venous valve function
- enhances lymphatic flow
- reduces tissue edema
- improves the microcirculation that enhances skin healing
- reduces lower extremity pain
Ssummarized from LEG ULCERS, Third Edition by David Negus et al. (editors). Hodder Arnold, Oxford University Press, 2005.
Cochrane database investigates whether compression stockings are beneficial ...
The Cochrane database investigates the utility of compression stockings in patients who DO NOT have an active venous stasis ulcer and in patients who DO NOT have a healed venous stasis ulcer and reported that :
- The symptoms subjectively improved with the wearing of stockings across trials that assessed this outcome
- There is insufficient, high quality evidence to determine whether or not compression stockings are effective as the sole and initial treatment of varicose veins in people without healed or active venous ulceration, or whether any type of stocking is superior to any other type
As such, they recommended randomized controlled trials (RCT) to investigate whether patients with "varices either wearing or not wearing compression stockings to assess the efficacy of this intervention".
The study is reported by S Shingler and colleagues in Cochrane Database Syst Rev. 2011 Nov 9;(11).