What Are Varicose Veins and How Are Varicose Veins Unhealthy?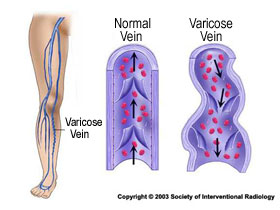
If you experience bulging leg veins, aching and pain in the legs, heaviness, tiredness of the legs, itching and burning along bulging veins, restless legs or leg swelling, you may have symptomatic varicose veins that warrant evaluation and treatment.
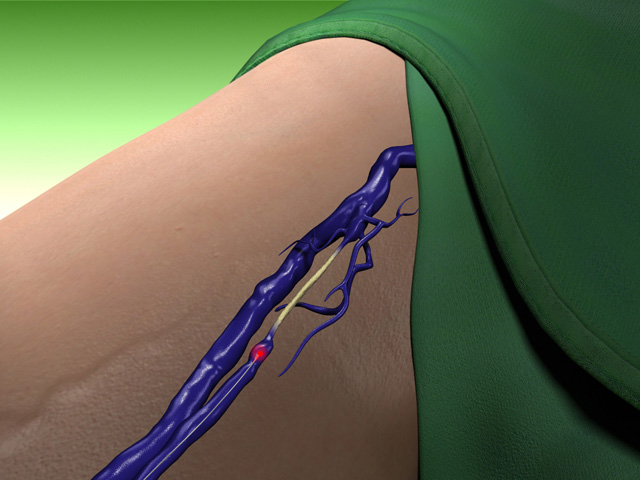
Varicose veins can become enlarged and in some cases quite prominent. They can be seen in some individuals as serpiginous (snakelike), raised lumps in the thighs, legs, calves and ankles.
The first reference to the treatment of varicose veins is credited to Hippocrates in the 4th Century BC. He used a "slender piece of iron" to traumatize varicose veins and thereby cause clotting of the vein. Another description is of historical note with removal of a varicose vein in the Roman Consul member Caius Marcus by Plutarch - of note, no anesthesia was used and when the surgeon went to do the same operation on his other leg, he is noted to have said " I see the cure is not worth the pain". Things have changed a lot since that time and the procedures done today are done in the comfort of an office setting with little or no discomfort!
The major superficial veins in the lower extremities include the greater and lesser (short) saphenous veins. Other veins include the superior epigastric vein, superior external pudendal vein (groin area), posterior arch vein, anteriolateral branch of the greater saphenous vein, anterior tributary vein and dorsal venous arch. As well, the posteromedial vein, vein of Giacomini, intersaphenous vein and posterior lateral tributary veins. All of these veins and their branches can become varicose.
I often remind my patients that the only place in the lower extremities where a vein should be visible is near the inner ankle bone (medial ankle), where the skin is thin and almost everyone can see the saphenous vein cross it as it heads toward the upper body. This is seen in children and teenagers and is normal. However, any other veins that develop as we get older are ACQUIRED veins, that is they are not present when we were young but develop as we get older! As they become varicose, the overlying tissues can get inflamed and the skin can change color once blood seeps out of the veins and stains the fatty (subcutanous) tissue and skin. These hemosiderin depostis are responsible for the bronzing of the skin which is most likely at the most dependent part of the lower extremities, farthest away from the heart - the lower legs and ankles.
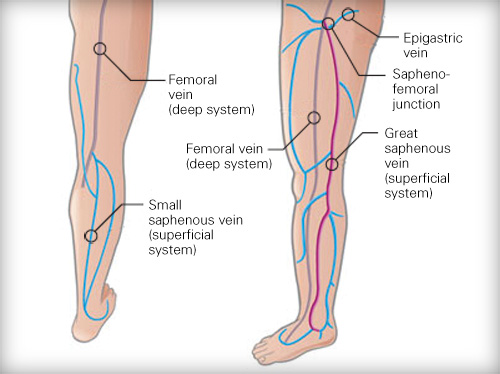
image of vein systems in the leg, image taken from westsussexveins.co.uk on July 25, 2010
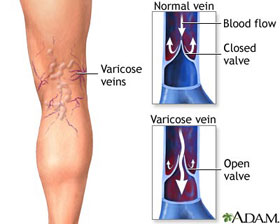
When they become prominent, they can be seen through the skin and may develop a purple-blue hue. If the skin over the varicose vein ulcerates, occasionally bleeding occurs from the thin walled vein. This can be quite dramatic.
More commonly, however, once the diameter reaches 5 mm, varicose veins cause itching, burning or an ache in the affected leg. This is especially notable when the individual is upright for several hours during the day.

image taken from gvg.org.uk on July 25, 2010
If the condition is left untreated, the skin overlying the vein hardens (gets indurated) and hyperpigmentation of the skin sets in. This is followed by swelling of the lower extremity. The final step in the pathophysiology of varicose veins is ulceration of the skin.


image of thrombophlebitis of branches of great saphenous vein, taken from Adam.com on January 11, 2008
Watch video clip of phlebitis (superficial vein thrombophlebitis) after microphlebectomy:
Chronic venous reflux disease, both originating from the saphenofemoral junction, saphenopopliteal junction or along perforator veins can lead to the development of venous staisis ulceration (see video clips)
WATCH THIS
VIDEO about Venous Stasis Ulcers
Watch the most downloaded video about venous stasis ulcers on YouTube - by Dr. Karamanoukian
Even in these latter stages, there is significant benefit to be gained by radiofrequency ablation of the varicose vein or phlebectomy.
How Do You Diagnose And Evaluate Varicose Veins?
 Following the history and physical examination, the next major diagnostic step is the ultrasound examination. The ultrasound examination gives us a real time and detailed view of your varicose vein system. Next, we prepare a comprehensive "venous flow map," which illustrates the path of the blood flowing through the abnormal veins and where the trouble begins. Special attention is paid to the perforators and the saphenofemoral junction for reflux disease.
Following the history and physical examination, the next major diagnostic step is the ultrasound examination. The ultrasound examination gives us a real time and detailed view of your varicose vein system. Next, we prepare a comprehensive "venous flow map," which illustrates the path of the blood flowing through the abnormal veins and where the trouble begins. Special attention is paid to the perforators and the saphenofemoral junction for reflux disease.
Patients are often surprised to see how extensive and complicated their varicose veins are and how superficial they are beneath the skin. This veon map that we create depicts details not visible from surface examination of the skin, that is, details that make treatment more effective.
Since each patient and each patient leg (right and left) are uniquely different, the vein map helps us configure the optimal plan to eliminate abnormal and varicose veins.
How do you treat Varicose Veins?
There are several treatment options for varicose veins available.
 Treatment options include:
Treatment options include:
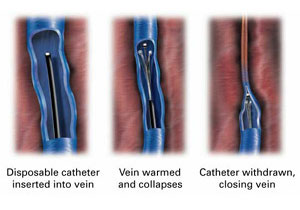
The VNUS Closure procedure treats the underlying cause of varicose veins, namely saphenofemoral reflux disease (commonly known as venous reflux disease).
We also have the most advanced laser vein system for EVLA to accomplish the same goal as VNUS Closure.
What Can I Do To Prevent Varicose Veins?
Many of the things that seem to cause varicose veins are difficult to avoid such as a family history or a sedentary way of life.
Whenever possible, avoid standing for prolonged periods of time. Walking is much better for the veins and helps blood return to the heart more efficiently, preventing the pooling of blood in the legs.
In professions or occupations that require extended periods of standing, a few steps should be taken at regular short intervals to help the venous circulation. These include things like wearing support stockings. No supplements or drugs are effective in preventing the formation of varicose veins.
What About Elevating The Lower Extremities?
If you are sitting, leg elevation at or near the level of the heart can significantly alleviate symptoms of leg pain and swelling.
Other things that you can do include:
- Showering with cold water if at all possible
- Use of compression stockings
- Losing weight as this is shown to reduce saphenofemoral reflux (venous reflux)
- Avoid prolonged sitting and standing