What Are Venous Stasis Ulcers and How Are Venous Stasis Ulcers Treated?
According to the American College of Phlebology, epidemiologic studies have found that the prevalence of venous stasis ulcers (leg ulceration) in adults, either active or healed, is about 1-2%. This is quite a number, suggesting that there are some 3 million to 6 million adults in the United States with venous stasis ulcers (venous ulcers). Depending on the study, venous stasis ulcers are 1.5 to 3 times more common in women than in men. They occur rarely before the age of forty and are found in as many as 3.4 % of patients older than 80 years of age. Venous stasis ulcers have been diagnosed and treated in patients as young as 20 years old!
In our practice, a recent survey and analysis of our database of patients with venous stasis ulcers was notable for patients treated as early as age 26 and as old as age 86. The vast majority are in the 4th decade of life and associated with a significant family history of venous insufficiency. Venous insufficiency is also called venous reflux disease and can originate at the saphenofemoral junction, saphenopopliteal junction, or along named perforator veins. A large proportion of patients (64%) recall a family member who had trophic changes in the legs, whether they were pigmented and brown discoloration of the legs (bronzing, hemosiderosis) or with a history of venous stasis ulcers. This is not an uncommon finding in patients who have venous stasis ulcers. Three out of 4 patients in our analysis state that they were told for many years by their physicians that "nothing can be done for the discoloration of the skin"! Nothing could be farther from the truth. Ask The Vein Experts at VeinsVeinsVeins.com
Venous stasis ulcers should not be confused with ulcers related to arterial insufficiency (peripheral arterial disease, PAD) which are due to inadequate flow of oxygenated blood (red blood) to the tissues. Peripheral arterial diease causing arterial ulcers are from advanced atherosclerotic disease in the arterial system of the lower extremities and are associated with diabetes, older age and high cholesterol levels (hypercholesterolemia) among other causes. Venous stasis ulcers are 5 to 7 times more common than arterial ulcers associated with peripheral arterial disease (PAD). The location of arterial ulcers are different than the location of venous staisis ulcers as the image below demonstrates.

This is in sharp contrast to the two images of venous stasis ulcers shown below:

Watch videos about venous stasis ulcers by Dr Karamanoukian (see below)
Watch this Dr. Karamanoukian video about Venous Stasis Ulcers >
Watch this Dr Karamanoukian video about healed venous stasis ulcer and lipodermatosclerosis >
&feature=related
Watch this Dr Karamanoukian video about venous stasis ulcer and lymphedema >
&feature=related
Watch this Dr. Karamanoukian video about venous stasis ulcer and perforator vein reflux >
Watch this Dr. Karamanoukian video aboout about multiple healed venous stasis ulcers >
Watch this Dr. karamanoukian video about sclerotherapy and venous stasis ulcers >
http://www.youtube.com/watch?v=KTLyG9PqyIU
Watch the most downloaded video about venous stasis ulcers on YouTube - by Dr. Karamanoukian - it has been viewed over 19,000 times as of 8-01-2018
Venous stasis ulcers are not only debilitating but costly. In one U.S. study, the cost per year per patient with a venous stasis ulcer exceeds $ 40,000. The total impact on the healthcare system is over 1 billion dollars per year. I have evaluated patients who have lived with a venous stasis ulcer for 20 years! Although this is not a common occurence, typically patients come to see us after they have failed to get adequate treatments by their primary care physicians or by wound care centers. A large number of hospital based wound centers espouse expertise in wound care and in most cases, lack an understanding of venous disease.
Very rarely are patients able to work as these open wounds require constant care and cause significant disability. Over 80 % of patients with venous stasis ulcers have limited mobility. According to studies reported in the medical literature, in terms of quality of life, the open wounds cause more concern for patients than symptoms of pain, itching, anxiety, social isolation and reduced ability to perform their daily routine. At least, these wounds require daily or twice daily wound dressing changes. In advanced healthcare environments and systems, patients with venous stasis ulcers are seen by home health care nurses at least once weekly. Physicians who are specialized in wound care also supervise the evolution of these healing wounds once monthly and more frequently when they are infected or have significant necrotic tissue. Dr. Karamanoukian has the experience to recognize and treat infections that are contributing to poorly healing or non-healing venous stasis ulcers.
At the Vein Treatment Center, Dr. Karamanoukian has developed special expertise in treating patients with venous stasis ulcers. Community physicians in the Buffalo Niagara Frontier and as far away as the Southern Tier and neighboring Pennsylvania have come to recognize this regional expertise and have referred hundreds of patients for treatment. The care of these patients is individualized and customized and is often multidisciplinary, drawing in the expertise of infectious disease specialists, wound care specialists, hematologists, endocrinologists and a Board Certified Phlebologist (Dr. Karamanoukian). Our success rate in healing chronic venous stasis ulcers in unparalleled in Western New York and Pennsylvana. A multidiswciplinary team is paramount to the Center of Excellence approach to treating patients with venous stasis ulcers. We use low level laser therapy (LLLT) to help heal venous stasis ulcers, Unna boots, wound debridement and refer patients, when appropriate and ready, for electrical stimulation therapy.
It seems that venous stasis ulcers have been a problem for thousands of years! Of note, the first description of treatment for a venous stasis ulcer was found in the Papyrus of Eber originating in Egypt from1550 B.C. According to Dr. Olle Nelzen of Skaraborg Hospital, Sweden, "four paintings show miracles performed by Saint Carlo for patients with venous stasis ulcers" in the Milan Cathedral in Italy dating to the 17th Century. It seems that venous ulcers were of public concern three centuries ago. The paintings by Giovanni Battista Crespi depict a scene where Aurelia Degli Angeli called on the Holy Archbishop Saint Carlo to heal a painful and odorifous ulcer in her leg which had been bothering her for three years! These pictures are hung at the Veneranda Fabbrica del Duomo di Milano and are quite a sight to see. Dr. Karamanoukian and his staff made a trip to view these painintgs (in 2007) while on a humanitarian medical mission with the Hope for Tomorrow Foundation.

A variety of etiologies can cause leg ulcers, but the majority of patients with venous stasis ulcers have venous reflux disease. It is estimated that venous reflux disease is 5-7 TIMES more common than arterial insufficiency, and can be considered an endemic disease.
WATCH THIS NEW VIDEO about Venous Stasis Ulcers by Dr Karamanoukian
Despite the prevalence of venous stasis ulcers, they are often neglected and inadequately and improperly treated. Patients often present to our facility with a 2-3 year history of having such ulcers and consider them as non healing or slowly healing wounds. One particular patient which is profiled on our YouTube video had a venous stasis ulcer for 20 years! She was being seen by a vascular surgeon on a weekly basis for years and literally nothing was being done to help heal this ulcer. A totally unacceptable treatment from the perspective of a Board Certified Phlebologist.
A very detailed and thorough history and examination is performed to rule out comorbid conditions that contribute to the poorly healing or non healing wound. These include conditions such as thyroid disorders, diabetes, kidney insufficiency and failure, among others. As well, coagulation factor disorders are sought out and investigated by special blood tests. The spectrum of blood tests and coagulation factor studies is determined and individualized by Dr. Karamanoukian at the time of consultation. All of these studies are covered by medical insurance.
Toe brachial indices (TBI) are measured to exclude arterial insufficiency to ensure that an arterial cause is not causing or contributing to the non healing wound. In African Americans, sickle cell disease is excluded. In some cases, the tissue is biopsied to exclude vasculitis, which is an inflammatory or rheumatic condition of the small arteries and arterioles of the body. As such, we use a very systematic apporach that is individualized to the patient' clinical presentation.
image of ankle brachial index (ABI) measurement taken from daviddarling.info on January 11, 2009
Doppler studies are done to exclude the presence of deep vein clots and to look for venous reflux disease, axial or perforator types. Duplex ultrasound is considered the test of choice for detailed evaluation of chronic venous reflux (insufficiency) - it combines color Doppler flow imaging with B mode and pulsed Doppler. It is very well documented that Duplex scanning is the most reliable, cost effective and quick method to identify venous insufficiency and obstructive venous disease.
Most recent studies have documented that the superficial and perforating veins are involved in most patients with venous stasis ulcers and those with recalcitrant and recurrent ulceration after inadequate conservative treatment.
Treatment of venous ulcers can be frustrating for primary care physicians. Goals should be directed at keeping the ulcer infection free, absorbing any excess discharge, maintaining a moist wound environment, controlling diabetes and elevating the legs, among others. This requires a multidisciplinary approach.
Several researchers have shown that dressing changes lower the bacterial load in the ulcer bed. Silver sulfadiazine has been shown to almost reduce the bacterial load to acceptable levels to accelerata wound healing. It is a broad-spectrum antibiotic and does not cause pain. Saline-dampened gauze dressing changes also reduce the bacterial load in the large majority of wounds, but not as effectively as silver sulfadiazine. Povidone-iodine solution (Betadine) is believed to kill granulation tissue, which significantly impairs healing of these wounds and should be avoided.
New investigations have also looked at nonsurgical methods of improving the microcirculation in the healing wound. The use of low-intensity ultrasonic stimulation of venous ulcers has shown a significant improvement in the rate of wound healing and should be considered in patients with venous stasis ulcers. This increased rate of healing is thought to be mediated by stimulation of angiogenesis, leukocyte adhesion, and growth factor production.
Supplying compression, promoting activity of the patient and the involved extremity and managing the patient's medical problems is the cornerstone of treatment. Controlling the edema is a primary concern. Compression can be achieved via multi-layer compression dressings, stockings or mechanical pumping devices.

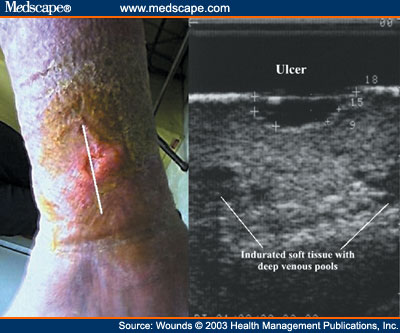
Sometimes we employ venous ultrasound to help direct compression therapy by identifying areas of the legs with venous pooling where compression stocking could best reduce venous hypertension and aid in healing the venous stasis ulcers. We do these assessments to help direct wound care specialists best help their patients heal their venous stasis ulcers (see below - image taken from medscape.com on January 10, 2009).
Since superficial venous reflux disease and perforator venous reflux disease is the underlying cause of a significant percent of patients with this disorder, endovenous ablation with VNUS Closure and VenaCure EVLA can greatly improve their prognosis. These techniques can also be used in very selective setting to obliterate perforator veins that are contributing to venous reflux disease in the lower legs.
There is strong scientific published data that shows that superficial venous surgery reduces the risk of recurrence of venous stasis ulcers within 1 year of treatment.
For more information regarding venous stasis ulcers and for a complete evaluation by a phlebologist, call Dr. Karamanoukian @ 716-839-3638.
If you have a venous stasis ulcer that has not healed and has been treated by a physician or physician extenders for more than 3 months, then you should seek an evaluation at the Vein Treatment Center and www.VeinsVeinsVeins.com
We will work with a wound care specilaist to optimize healing of venous stasis ulcers and have had very successful results with our directed vein procedures in healing these ulcers.
The Vein Treatment Center is a National Center of Excellence for Vein Disorders. Dr. Karamanoukian is listed in the 'Guide to America's Top Surgeons' by the Consumers Research Council of America. VeinsVeinsVeins.com is a highly rated and objective portal for information about venous reflux, venous insufficiency, venous stasis ulcers, VNUS Closure, EVLA, perforator venous reflux, perforator veins, varicose veins, spider veins and reticular veins.